The Aluminic–Neuroinflammatory Two-Hit Hypothesis for Autism
Could early immune exposures explain the rise in autism?
Abstract
Clinical and pharmacovigilance data suggest a possible link between early immune events and the onset of autism. This hypothesis proposes a two-phase model: initial exposure to aluminium from vaccine adjuvants, followed by a neuroinflammatory event that enables the entry of aluminium-laden immune cells into the central nervous system (CNS). This framework offers a coherent explanation for both early-onset and regressive forms of autism and provides a basis for targeted investigation.
Introduction
Vaccines administered during the first year of life temporally coincide with the period when initial signs of autism typically appear. According to the WHO’s VigiAccess pharmacovigilance database, vaccines such as MMR, DTP, Hib, PCV, hepatitis B, and varicella are among the most frequently associated with reports of suspected autism. This chronological overlap justifies the development of a specific explanatory model.
The Hypothesis
Autism may result from a sequential two-phase immunological process:
1. First Hit: Aluminium Adjuvant Exposure
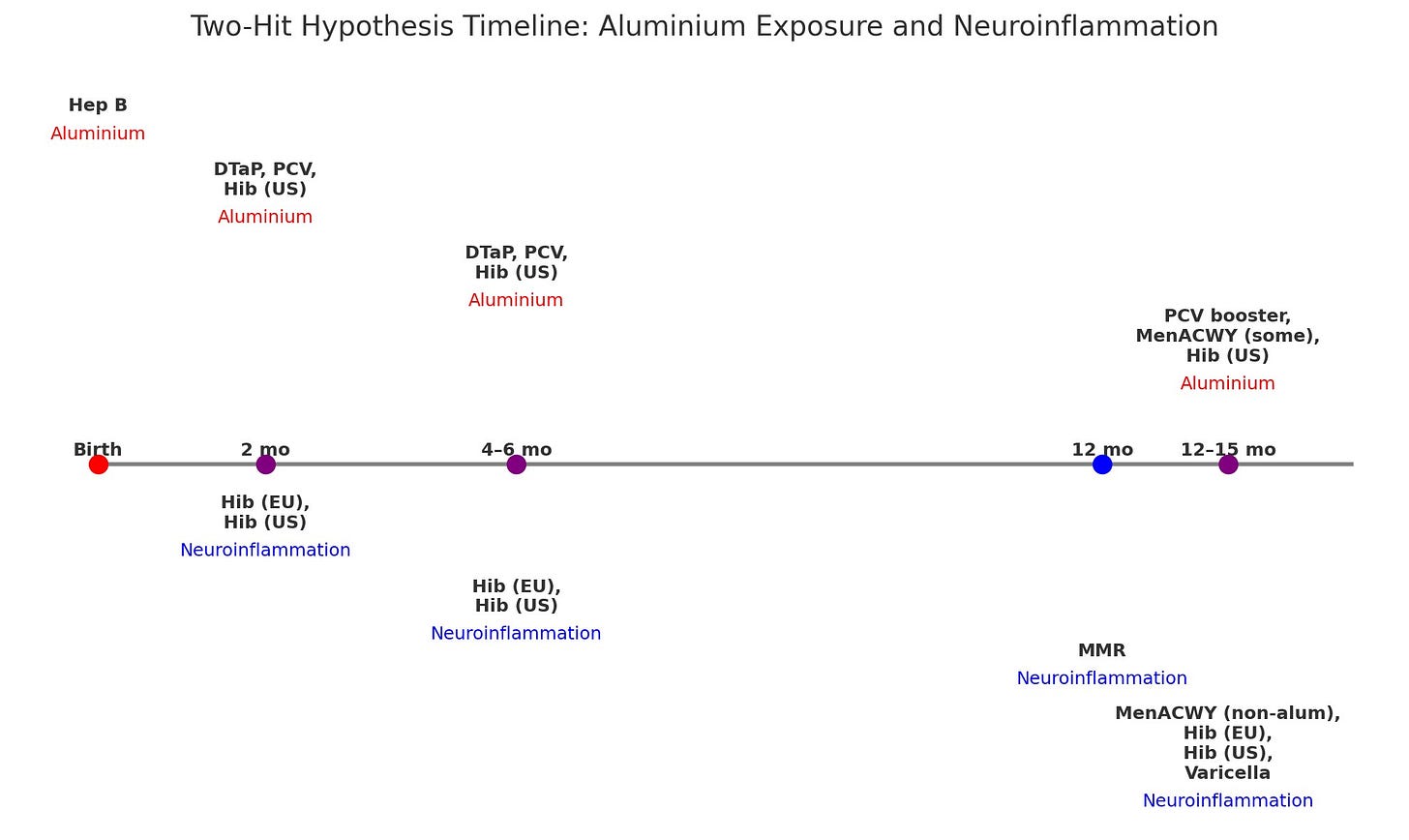
During the first six months of life, infants receive vaccines such as hepatitis B, DTP, PCV, and Hib (US formulation), all of which contain aluminium-based adjuvants. Aluminium is sequestered by macrophages and may persist in the body for extended periods.
2. Second Hit: Neuroinflammatory Trigger
This second event may occur as early as 2 months of age with conjugate vaccines (Hib, PCV, MenACWY) or later with live viral vaccines (MMR, varicella). These immunisations elicit robust immune responses that could transiently disrupt the blood–brain barrier (BBB), allowing aluminium-loaded macrophages to infiltrate the CNS.
This phenomenon may be exacerbated if, when receiving the MMR, the child is already immunologically activated due to an infection. That could make it easier for aluminum-carrying macrophages to enter the brain or trigger a stronger reaction there.
The possible role of conjugate vaccines as a neuroinflammatory trigger had previously been hypothesised in 2011 by Richmand (1), who proposed that these vaccines may overstimulate immune pathways during critical periods of neurological development, thereby increasing the risk of autism.
In addition, it is worth noting that the MMR vaccine, which has been occasionally associated with aseptic meningitis in post-vaccination surveillance, contains sorbitol as a stabilizing excipient. Sorbitol has also been implicated in cases of aseptic meningitis induced by intravenous immunoglobulin (IVIG) preparations in clinical settings. Although the quantities used in vaccines are significantly lower than in IVIG products, and administered via a different route, this raises the possibility that sorbitol—and potentially other sugars such as sucrose or lactose used in various vaccines—could contribute to a minor but relevant pro-inflammatory effect in the meninges of immunologically primed infants. This potential mechanism may help explain the neuroinflammatory component of the ‘second hit’ in the case of MMR and related vaccines.
Mechanistic Model
Phase 1: Immune priming through aluminium-containing vaccines.
Phase 2: Subsequent immune stimulation compromises BBB integrity.
Result: Aluminium-bearing immune cells enter the CNS.
Consequence: Local neuroinflammation may interfere with synaptic development and neuronal connectivity.
The plausibility of this mechanism is further supported by the work of Exley et al. in 2018 (2), who found unusually high levels of aluminium in brain tissue from individuals with autism, suggesting a possible neurotoxic contribution to developmental pathology.
Clinical Consistency: Two Autism Onset Patterns
The hypothesis accounts for two well-documented clinical presentations of autism:
1. Early-Onset Autism (Non-Regressive)
If the second hit occurs within the first months of life, neurodevelopmental disruption may manifest before core skills emerge. These children often fail to develop typical social and communicative behaviours.
2. Regressive Autism
If the second hit occurs later—such as following the MMR vaccine—it may lead to the loss of previously acquired skills including speech, social interaction, and play. This pattern has been extensively studied by Ozonoff et al. in 2018 (3), who explored variability in onset types across informants, methods, and time points, confirming the existence and prevalence of regressive trajectories.
“This dual-pathway framework lends clinical coherence to the hypothesis, integrating both early-onset and regressive autism under a single immune-based model.”
Conclusion
The Aluminic–Neuroinflammatory Two-Hit Hypothesis provides a focused and testable model of autism origin, based on the sequential interaction between immune sensitisation (aluminium) and later immune activation (neuroinflammation). The timing of vaccine administration, pharmacovigilance data, and clinical patterns of autism onset collectively support the rationale for further targeted research.
References
Richmand BJ. Hypothesis: conjugate vaccines may predispose children to autism spectrum disorders. Med Hypotheses. 2011;77(6):940–947. doi: 10.1016/j.mehy.2011.08.019
Exley C, Mold M, Shardlow E, Pickup J. Aluminium in brain tissue in autism. J Trace Elem Med Biol. 2018;46:76–82. doi: 10.1016/j.jtemb.2018.01.002
Ozonoff S, Gangi D, Hanzel EP, Hill A, Hill MM, Miller M, Schwichtenberg AJ, Steinfeld MB, Parikh C, Iosif AM. Onset patterns in autism: Variation across informants, methods, and timing. Autism Res. 2018;11(5):788–797. doi: 10.1002/aur.1943